Advertisement
Explosive Whistleblower Nurse NYC Elmhurst Hospital Speaks Coronavirus Covid-19 Pandemic Lockdowns
Explosive Whistleblower Nurse NYC Elmhurst Hospital Speaks Coronavirus Covid-19 Pandemic Lockdowns
https://www.youtube.com/watch?v=UIDsKdeFOmQ
https://www.webmd.com/lung/news/20200424/large-study-of-covid-19-nyc-hospital-cases-shows-high-mortality#1
- Category: Mass Mind Control,MartialLaw/Lockdown/StateOfEme,Vaccine / Mandatory Agenda,Virus / Bacteria / Sickness
- Duration: 01:18:09
- Date: 2020-06-11 22:49:35
- Tags: coronavirus china wuhan outbreak pandemic lockdown quarantine
7 Comments
Video Transcript:
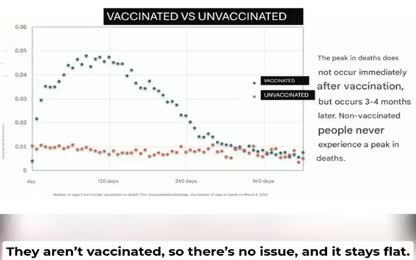
you put it another way let's look at mortality those aged 18 to 65 years of age and those greater than 65 years of age those who are on no vent and those that are on the vent or had to be on the vent mortality rate for those 18 to 65 not on the ventilator was 19.8 percent those greater than 65 26.6 percent on the ventilator between 18 and 65 years of age 76.4 percent those on the ventilator greater than 65 years of age a whopping 97.2 percent mortality based on this data almost from the onset of the coronavirus epidemic in the United States New York has been described as the epicenter of the outbreak and Elmer's hospital in Queens the epicenter of the epicenter of the epicenter of the epicenter of this crisis here in the city and in the country with doctors desperately trying to keep up with the growing number of patients as well you see the black body bags you say what's in there it's Elmer's hospital must be supplies it's not supplies it's people also from the beginning of the crisis ventilators were described as essential life saving equipment initially in short supply you pick the 26,000 people who are going to die because you only sent 400 ventilators I knew that every person who needed a ventilator and didn't get one would die but why does New York and Elmer's in particular appear to have been hit so much harder in other places in the United States and were ventilators ever the right approach to treating COVID-19 especially once we realized that 60 to 90 percent of those vented to not survive the experience and observations of nurse Aaron Olshewski seemed to offer some answers to these pressing questions while simultaneously providing frontline information about a number of other hot button topics including the disproportionate number of COVID deaths among Americans of color the distortions surrounding do not resuscitate orders the disregard for personal protective equipment standards and the clustering of COVID positive with COVID negative patients which she witnessed again and again and the tremendous amount of nosocomial or hospital acquired infections that resulted perhaps most urgently of all she speaks of the therapies and protocols employed in her home state that did work Aaron was brought from Florida by a service funded by the Federal Emergency Management Agency she spent almost a month at Elmer's which she saw there compelled her to become a reporter and whistleblower alongside her already extensive nursing duties she made recordings posted warnings on social media and spoke through proxies about the night-american dish and she witnessed Aaron was raised in Wisconsin and enlisted in the Army when she was 17 just before 9-11 she deployed in support of Operation Iraqi Freedom in 2003 part of her duties involved overseeing aid disbursement and improvements to hospital facilities while in country she received the Army Commandation Medal for Maritorious Service and was wounded in combat Aaron eventually retired as a sergeant and became a civilian nurse in 2012 a mutual friend who was helping her make hidden camera recordings introduced us to Aaron after working a long shift at the hospital she agreed to do an impromptu interview in her room at the Marriott Marquis overlooking Times Square we encourage the viewer to leave aside their preconceptions about the nature of what is happening to hear firsthand from an eyewitness who had great personal expense and without political prejudice of any kind now openly reports what she discovered in the hopes that the information will be put to good use to save lives she began by telling us one of her most disturbing findings that people who had repeatedly tested negative for COVID were being described as COVID confirmed okay so if you look close I'm in my patient's chart I am pulling up like their laboratory results so if you look here you'll see COVID-19 BioRefrance Lab here are the test results as you can see 5-1-2020 at 17-16 not detected they test for a second time 5-4-2020 at 17-59 not detected so both of those are negative scroll up to the top this is my patient they are on event and they are being called COVID-19 confirmed droplet and contact eye and eye protection so this person is droplet and I COVID confirmed has it a click not detected no result in that reveal well Aaron was using her hidden camera to document another chart showing a patient with negative test results who nonetheless was labeled COVID confirmed another travelers entered the room they began to discuss what Aaron was seeing so not detected here but it's not detected so you said that they were vented immediately upon being brought in is that yeah so the thing is they're coming in with difficulty breathing and a lot of these patients are really coming in with anxiety because everybody is scared and when I was back home I was working in the ED out in the tense and most people that were coming through were coming through with symptoms of anxiety or they're worried and they're breathing fast and they get all nervous so this is how the people are like coming in now I'm not saying that some of them you know don't have COVID like there are there is there are people that come in and they really do need help not to the extent of the event but they need help but these other people like this person who wasn't COVID multiple times you know in a lot of them are on either medicaid or medicare they're poor they're from you know a lower class we're at a public hospital they need the funding so take them they take them and they tell them pretty much that if they don't get on event then they're probably not going to survive what the reality is if they get on that event the likelihood of them walking out the hospital is symptoman and can I ask you what like peep are they on and is that being mandated or specified what the pressure is on the event? Here's the thing with this so you don't have actual doctors that know critical care ICU doctors on these floors there's a dentist and there are residents with these so residents are essentially students and they have no idea what they're doing like I had to police actually today I had to police a resident because he wrote an order for me to run Versed which is a medicine that you have to be very careful with because it can kill someone at like quadruple the speed of what you should be running at the dose and had I not known that then I would have easily killed the patient and it would have been okay under their COVID standards so everything is kind of a wash nobody's held accountable for anything and these people of our infants are essentially being like they're these residents are like practicing their skills on them so they're practicing central lines they're practicing like invasive procedures that are really unnecessary what is the percentage of black Latino white what what's the racial composition? Hispanic and black for the majority and what's the age range and Asian and what's the age range? 20 year olds all the way up to 70 80 year olds very very few out I should say very few 80 year olds but the majority of people I would say are in their 40s or 50s Wow and what percentage of the people that are in there deep would you say actually have tested positive for COVID? 1,5 really half but everyone is being treated as though the entire hospital is COVID so I have to hospital is not COVID but there wasn't COVID floors so let me just ask you about nose acomial infection so you're saying they're putting non-COVID or COVID rule out with definite COVID patients yes so I was only wondering because I was looking at like all the patient rooms and like this patient is in with like a non-COVID and I don't understand what they're doing I know there's four patients in a row here in a non-COVID and this is supposed to be the COVID because seven floor they shut it down and they're going to have non-COVID there this is going to be the only COVID so they shouldn't put any non-COVID here they're going to say they've been doing they're banking on the fact that they'll get it because they're already immunocompromised so they're just and they'll put them in the same room so there's double rooms so you have a COVID with a non-COVID they don't even care we have enough rooms where they can be separated now because it's not as busy as it was you know four weeks ago but they don't care they're just putting them together I have that right now happening and like the guy over in the end of positive like the guy over in 29 I had him upstairs on cc before it yeah and he came in with a stroke I know that's what 261 was a stroke and no COVID and now he's got COVID and he's on event because we gave it to him here I don't know how this doesn't be moving so far I know but she literally came in with a broom and then she left like five minutes later the patient had died of COVID and she didn't lock the poor she was cleaning getting prepared for my next patient and she didn't lock the poor what? I was like that is the way to stand there I didn't think I had to tell her about it people don't know how to properly wear their PPE let's go back to Ebola like when Ebola was here people took that very seriously you have a you have a nurse in the room in all the head to toe PPE this is Ebola this is I'm going to compare it and you have another nurse that's outside the room handing supplies the clean nurse and the dirty nurse right going and when they're taking their outfit off the one nurse is unzipping the back so she can take it out walking out they're not doing that here we're wearing like our scrubs and then we have maybe like a net top our pants are exposed they're wearing booties over their shoes but the booties are going room to room to room and then people will wear them through the hospital so there's massive spread just through the improper use of the PPE I mean that's it's a no-brainer everyone it looks good it looks good looks like you're super safe but in reality it's ridiculous you're going to go to your go room to room and maybe take that top up and a new top on but the rest of you are still exposed but I mean why are they doing this you know suspected suspected and then there's like responsible hospitals that mean they can like a nose economy old is that what that means? like we have in the United States and we've had it for a while a rapid test that's 45 minutes do you have COVID doing you? they're not they're not doing the rapid test here they're not okay I don't know if you've never seen them nope they don't do it it's too expensive they do five days it's like five to seven days turn around in the meantime they admit them on to COVID units so non-COVID the rule out are going to COVID units and waiting for the results even though we have a rapid result which is 45 minutes and they're not doing it no not one but would you say it's too expensive I mean isn't this all getting charged to the fund anyway? I mean why not do it? why not? are you saying that? I don't know why it doesn't make any sense to me I asked that doctor what's the opinion about it? how come you guys don't do the rapid test here? I see the place I mean it exists it's just they don't have access to it it's only limited supply so if you have deep pockets you get first oh so money? most times it's money about everything yes that's sad it's the reality I compare this hospital to a third world country I've been in a third world country hospital in Iraq the Iraq hospital is better than this one and that says a lot I've been there I've had I've been in both hospitals and we're this is in the United States in this hospital is treating low income mostly people and it almost makes me feel like I think these people are disposable and they're not they're people you know everybody people are not disposable you know especially especially these the ones that are struggling day in and day out the hard workers you know like trying to reach that American dream and they're not giving a chance they're brought to this place where nobody cares and is there a understood financial incentive to diagnose COVID? yeah of course so in the hospital that I'm in right now it's all COVID at this point every single floor is COVID and they needed that way obviously for a reason in my opinion but a person cannot come to the floor unless they have a COVID diagnosis did this the reason that they not want to cross contaminate is that would that be the legitimate reason why you would create an all COVID floor? um here's why I will say note of that is because they're admitting people for quote quote COVID rule out so this guy was probably admitted COVID rule out tested them they saw that it came back negative they probably already did something where they needed to now call him COVID and then the hopes that if they're putting him on a COVID floor and there's nurses going room to room to room he will get it and then they'll be you know they'll be back when he does pass that he did have COVID yeah I mean that's that's quote they know that's quite a charge I mean what makes you think they really want them to get COVID because it money money it's I think it's at least $29,000 per patient and then you have to think you're also charging supplies and more supplies and more supplies that's just like a bonus money but what did the but the residents aren't getting that right well that's the thing and I actually had a I've went at it with a lot of residents already they're order followers so there was residents and I have this on tape I vide taped it because it was just so disgusting to me a 37 year old which is my age was not a DNR it's a full code his family in depth discuss with the doctors that they want us to do and they can to say him he came in talking he was very terrified he was just like you know totally alert knew it was going on and they convinced him to be on a vet now he's dead but the doctors said when I turn into shift that if he codes that we are not to resuscitate or try to save him and we flipped this is important I just asked them to put a DNR order on they said no that's up to the funding so we're going to hold now that's what I said and they said no one asked us we are obligated to so that I got to say something though like it's our license unfortunately you guys got to put it in order just something that's what I said I said I'm obligated what did she say? so that she's like the higher up said I said I don't care what they said when higher up god we don't have a god here making this decision so I said I don't care what they said so we're supposed to he's not DNR but we're treating it as you know basically because his family know his family knows the situation they think they call them and they told them they were trying to see what people can do in town all days spent like in the 80s saturated it was this one on the forehead it was this one work and when I changed the order oh it was 90s so they started playing around with the next one so they started playing around with the next one oh shoot it's 90s he changed the pulse act from his head his finger he went go the one hand he's so sorry so so what was that? so that was we were just getting on shift because we were starting the night shift at seven and that was the nurse from the day shift saying pretty much we shouldn't code him if he's going to code and then I turned my glasses on where are we being told not to to code him especially but he said I mean because I'm going to tell you right now keep on him's out I'm jumping on his chest period point blank it's going to happen because until that status is changed in the computer that's what I'm going to do under minor single right I mean um uh because you guys are going to pack me up and protect me well Elmer's does have a policy given like a coded policy giving the scarcity of dialysis blood it can be a cancoded can be whatever it's not there's not a it's a difference normally the standards whatever the family says like we just do um it's a little bit different now because of the new policy in place the dark room in place which is that you don't need full family it's like you can just tell someone that it's met up with Utah and we're not willing to just pour blood and resources into some of them would be a possibility to back but I look it's 3037 I mean it's good they tried well our higher ups have agreed and our attenings agree that this is due to how care at this point he's actually I said he doesn't have an attenement going he doesn't have anything to sustain going and I said who decided this and I said can you put a comfort care order in that no we can't do that can you put a dn or order and no we can't do that I said so what's our plan do we have a policy well he's dying and I'm like I understand that but there needs to be an order indicating that either i'm doing compressions or i'm not doing compressions well I can say that we can all be an agreements that we will do it I will definitely because I'm going to jump on so why I'll go right with you I don't care that's what we that's what we're here for I'm not like I totally changed his status that he is a dn on and they can do a true position consent if they've talked to the family but until they change it and I see it he's a full coat to me what if we know when someone is we're close we'll pull the cold card up and be ready you know we're ready I had the appy ready that's one of the first things we do and she wouldn't let me give it so this was that woman in the entire time and this was over his over his body his alive body and we're arguing and she's laughing she was smirking and how that how this this man died was the nurses arguing with the doctors over him as he was dying and she's smirking the entire time I was a soul it was probably one of the worst experiences in my entire life but all I can think about is that at least he knows that we were fighting for him when he died you know but this was my conversation after after what happened and the guy I told you about earlier that had pulled his tubo he was up at that point like he was on the same floor he had pulled his he was the one that they wanted to sedate so at that point he was doing better where he could walk and put a diaper on him and told him to poop in his pants so after the cold I wouldn't go check on him and he's pooped he has peels I have pooped in my pants and he said that because the doctor told him that he has to do that and I just lost it it was her this is wrong it is straight up it is wrong and I have been I have 37 years old I have been in a hospital since I've been 16 military hospitals that well I agree that there were parts of that that were wrong too calling a patient a DNR when there's no order for it and telling us like straight up telling us you're not doing anything that's wrong if that was my brother or my father or anybody I was just a little bit furious and I guarantee you if I called his family right now and told him what happened they would be furious too I flipped we were all crying there's a lot of nurses that were that know that this is wrong but they're afraid to like say anything publicly she said when I was talking to her she said we don't always give him orders it comes from the top down and I was thinking that's the exact problem with everything that's the purpose you guys really try to kill everybody and like everybody thinks within our unit it was a big fight and ultimately the kid died with us over his body arguing about this and the doctors the he's like the doctor would just break it up that we you know I don't know I'm sorry I'm not doing that the doctor that came upstairs that I had worked with prior he was working in the ED heard out what happened he came into the room with me and told me that what I did was good and then you know so there are good doctors in here you know I guess the word traveled after this you mentioned earlier that this is a common occurrence where people come in able to speak and they just have what low oxygen levels and then and they're put on event is so what's what's what's going on there I don't know I honestly I have no idea how they're assuming everybody is just the same there's no individuality anymore these residents I think a lot of them are just stone cold you know there's no emotion and they don't view people as people anymore and it's really sad like weekend I came a little bit later you know after the big rush but there was still a lot of people coming in and a lot of us were just in shock within the first couple days you could see exactly what was going on my bigger problem with this whole scenario is when they intimate people they don't need it yeah and it looks very clear to me that they're just pushing it you almost feel like you're literally living in the twilight zone and you feel like you're the only sane one in the bunch of insane people and it's scary because these are people that others are trusting to take care of them and they're really doing the opposite I'm to the point where I'm afraid that I'm going to start thinking that this is normal I don't want to ever get to that point because they think that like the people I work with that are local nurses and doctors don't see anything wrong with us really I mean they don't really see this is just like kind of a hard past few months this has been like this and from what I hear like from I mean there are really there are good nurses that work there too like I have made good friends with a lot of the nurses that do work there there's good people but they're outnumbered so what happens people come in like this 37-year-old and what was he complaining of or what was going on respiratory distress he didn't have COVID either he did not have COVID and how do we know that? I took care of him I have the same type of results from his chart as I do with my other patient it was like the day before intubation who was fine on their own breather and then he got on the wall and then he got on the tube and now he's 37 years old and that's what I'm seeing like all these negative tests and they're putting them on these fence it hopeful that they'll get it they'll be put on these COVID floor is murder it straight up is it is studying these people up for failure based on money Medicaid is who pays out or who's paying this bonus of 29,000 I believe it's Medicaid Medicare it's government money but I don't know exactly where it's coming from I know that it is but I know that orders are coming from the above someone above and everybody says that it's someone higher up I'm like good call them like during that DNR when they're telling us or the full code when they're telling us not to you know do CPR I'm like all right call your higher ups then let's talk about it and they wouldn't care everybody's scared and everybody's scared to stick up for themselves and I've called a lot of doctors unethical to their face and they deserve it I am a nurse I'm an advocate for my patients and to but no no no this way you were laughing and you thought it was funny you were like smirking you've been really rude to all of us and I thought that was really to it was really yeah you are it was very disrespectful and I don't think that you're going to be a very good doctor you're welcome I hope you learn something from this Was this the dentist or are these her residents you're talking to this one was a fellow she was a CCU fellow a career she's a career fellow what killed him was being did the vent kill him yeah oh yes they're so sedated he had probably eight or nine drips it's all sedation it's all sedation and paralytics so you are asleep it is essentially like you're under you know you're in surgery you know when they put you under like that for a good month straight there's no way you can recover from something like that you're being dead if you do so can you list some of the drugs that they're put on on the drips? yeah there's propa fall fentanyl, nimbex um versus gosh here you go and I have a list I think it lists from this is one of my patients with on this just one patient so nimbex 100 milligrams presidx 400 milligrams fentanyl 2500 micrograms heparin 25,000 units versus 50 milligrams leave a fed 16,000 neo 50 milligrams propa fall 10 milligrams vessel press in 100 units this is one person and they're all these drugs are running at the same time into them so in the case of this 37-year-old he comes in complaining of some respiratory distress could he have low blood oxygen? totally healthy guy and he was satting like a such like that's the oxygen saturation and like 88, 89 so a little low I mean yeah but people do that we're not monitoring our oxygen you know all day long but he felt shortness of breath so he came in and what was the next step? what would have happened next? um he went to a stepdown unit um among other what does that mean sorry? it's just a unit that where people aren't quite on the vent yet and I stay on the vent yet because that's I should call it step up unit to the vent so was he can do they what's the phrase he used? COVID rule out so that's how they admit everyone to the floor that doesn't have a positive COVID immediately okay so he's put in the step down unit which is a euphemism for step up unit and what happens to him there? what's going on there? um oxygen I wasn't in this unit my friend was so just normal oxygen nasal no they'll do like a high pressure um so what does that mean exactly? it's pretty much like a forced it's a big it almost looks like a big thick nasal canyelon you put it in your nose and it forces the pressuring it can almost be like you know it's still causing your lungs to expand right but what they really need to be doing is like the non-rebrea their mass but they just skip it usually high pressure so their lungs are already you know so and tell just tell us what a non-rebrea their mass is so that's just there's a big a bag that is on the end of these masks it's not 14 air down your lungs okay it's more than enough okay um you can put a 100% oxygen and that's what people need that okay so and and that really is not the protocol it's not the protocol to start people on that I mean it should be but it's not how they're doing that now I mean in in your prior experience dealing with people with low saturation would that be what you would do? oh yeah that's what we were doing you know and my my hometown and were you having better outcomes there? we didn't have this because we treated them properly you know what was what would you say the kind of the case fatality rate was 9-0 yeah by me 0 and what's what what is the likelihood of coming out of the hospital you're in? I'll tell you that the unit that I've been on the only person that survived ironically is a guy who pulled his own uh two-bow so he woke up enough to be able to do that? yeah he wanted it out he should never been on the first place that's another that's a whole mother story so let's just keep going with this 37 year old so he's on the step down unit and he's being given sort of semi-pressurized oxygen it's not a rebreather mask and then what happens to him? they'll start treating them with medications you know that will I and are they checking his saturation at this all the time does he have? yeah he's on a continuous pulse ox but you know the minute that he desacts like they'll see like oh no he's at 87 now or oh look at this oh he's gonna need more help and then they go tell them that they need more help even if they don't you know it's ultimately what it comes down to is like people being just lazy and wanting to treat they just want to treat treat treat treat you know is there any incentive to the okay you're saying that the incentive for the residents is kind of experimental almost um was there order followers? you know like they want to please that's what they're doing and they want to please and like the protocol that hospital is to treat to treat in invasively according to this protocol and do we know where this protocol originates? I mean because obviously the governor was talking about getting vents vents everyone was talking about getting vents so this seems like this comes from very high up yeah I mean if you're gonna tell somebody they interwalt the entire world essentially and especially the entire United States when they're like we need the vents like if you tell people something enough they're going to start believing it so that's exactly what happened tell me what kind of immediate we thought two months ago that they need 30,000 heads how do you just come up with a number of companies that idiot too well I don't think medical is saying that oh yeah 29,000 okay so our 37 year old went what happens to him next so they say okay it looks like he's at 87 he needs more and so they do they that is that the point at which they would intubate him? yeah that's when he went to the that's when he stepped up so he stepped up to the ICU he steps up to the ICU they start off with a little bit of also relaxer and you know he's woozy you actually remember there's no family with these patients so they're alone and in hospital by themselves during a pandemic that they're terrified of already is probably what brought him in the first place totally healthy otherwise and then you have doctors they think they're doctors but they're they're resident technically with an absolutely zero experience. I've had to teach residents several nursing skills. Telling them that they have a choice, you know, like they could likely die from this, or they can be saved by, you know, getting a tube and that will help them breathe. They don't pull it down later. You can give you a little help breathing. And that's it. Then they get the sedation and they want, they go to sleep and that's it. They don't wake up. He's in a body bag. And so the drugs have a deleterious effect on the body, on the brain, but is there something about the pressurization of the lungs that is also causing harm? Yeah, they're having the pee. That's the pressure in his lungs, which is causing the sphero trauma of people, it's blowing people's lungs out. So when that happens, what are you going to do? Turn it up more. You just keep... Because the membrane expands so that you need it in order to fill them and deflate them, you need more pressure. Yeah, you're going to have to max it. I mean, we have a guy right now who's maxed on and everything. There's nothing more you can do. So then what? You just wait for them to die. I mean, there's nothing you can do. Can you tell us what peak levels are they started on? It depends. They're always usually... Well, they'll start... There's some good... I can't say everybody's bad. There are some good doctors that'll start them on on five, which people should be at about five. But that doctor goes home and the next doctor comes on shift and cranks it up. It's hard to go back down. And what oxygen level are they put on? It depends. I mean, as they start to deteriorate more and more, then the oxygen obviously is going up. There's a guy right now. I have a amount of 100 percent and I'll have to come in and give them a little bit more rush of two minutes of even more oxygen just to keep us that up. I mean, that's what happens to people. In your home state where you were treating people, what would the protocol be? I mean, it varied upon each individual, but we definitely would never go immediately to, you know, you're going to need a vent. You didn't feel pressure to diagnose people. People that there wasn't a pressure to diagnose people. COVID. Not at all. No. We're not a public hospital, too. That makes a huge difference. What I'm seeing is it's the public hospitals. And this is like in other states, too, if you look at out the hospitals, most of them are public. They're needing money. But our hospital would just treat them based on the individual, and they were using the hydroxychloroquine and the zinc and that protocol, for sure. At your hospital. And that seemed to work? Yeah. We didn't have anybody that died. I think there was one patient that was admitted and went home like the day later. And we're going to, I'm in a pretty big city, so. And were these people with, we were elderly with co-orbidities who were having good outcomes? Yeah, actually one guy, the one guy that was admitted came from a nursing home. And he was a wheeze, like a severely overbeat or a wheeze. And he left after a day? I think, well, I think it was like a night, maybe two nights max. And what do you remember what he was treated with? I didn't have him on the floor, but I can't, I can imagine he was treated with the protocol that we would prescribe the patients before the left emergency room, which was the hydroxychloroquine drink. Why do you think that's been demonized so much? Because it's working and then people wouldn't need friends. I don't know. Only on two tonight, a Houston hospital is having success treating the coronavirus patients. In fact, its recovery rate is perfect. Fascinating, isn't it? To treat patients here, Dr. Varan is using an experimental drug protocol. It's a cocktail of vitamins, steroids, and blood thinners. Each patient also is getting hydroxychloroquine, the malaria drug touted by President Trump. The protocol is controversial because there hasn't been time for extensive testing, but Dr. Varan says it works. We've treated over 40 plus patients with this treatment and we haven't had a single complication. So far, he says none of his patients have died. This is time of work, but it's no time to double blind anything. This is working, and if it's working, I'm going to keep on doing it. We're finding clinically with our patients that it really only works in conjunction with zinc. So the hydroxychloroquine opens the zinc channel, zinc goes into the cell, it then blocks the replication of the cellular machinery. You're prescribing it and it is working for COVID-19 patients. Every patient I've prescribed it to has been very, very ill and within eight to 12 hours, they were basically symptom-free. So, politically, I am seeing a resolution that mirrors what we saw in the French study and some of the other studies worldwide, but what I am seeing is that people are taking it alone by itself, it's not having efficacy. Okay. What can you tell us about any confirmed COVID cases that you've seen? I mean, both in your home state and here in New York, what have you noticed about them and what are their stats look like? Okay, so the real confirmed COVIDs that come in, you immediately know that they're COVID because they cannot, they can't breathe, they literally can't breathe. So they do need that, not to breathe their masks or their stats will like quickly drop to you know, 60, 70s. You want to do it around you know, 90 to 100. So they can't talk even? Some of them can talk, a lot of this is anxiety, but the problem with this is they're being told, the public has been told to self-quarantine, right? Stay home. That's a problem because these people could be getting early treatment. This clinical trials emerging that appears to show that it decreases severity early in the game before you end up hospitalized, before you end up on a ventilator. And they're not because they're told to stay home. So they're not getting really really sick and they come in on an emergency status. They waited too long and they didn't wait too long, they're easily treatable. And easily treatable you feel with some of these treatments. Yeah, like zinc and hydroxychloroquine and you know, any, yeah. It's work. I mean, it's been proven to work. There's a doctor I think in Texas that's you know, using that protocol and a shot in the butt, you know, of antibiotic, I don't know exactly which one she was using. And she's successfully treating. And she was saying that the pharmacist now is calling her every time that she prescribes, you know, the hydroxychloroquine and asking with the diagnosis was the patients in order to give it to them. Like that's a doctor patient relationship. So the pharmacist I guess was told to do this. And you know, in New York, the governor said, you know, pretty much put a ban on it. So why? Why? What made him, you know, a medical professional now to make these decisions and intrude on the doctor patient relationship. I think I know, you know, I've seen it. It's the one event. He wants to be right. They requested all these events. They want to use them. As part of the same executive order that granted hospitals near blanket immunity from malpractice litigation during the epidemic, Governor Cuomo singled out hydroxychloroquine as the one drug that could not be used as an off-label therapy for COVID-19, except as a part of approved studies. The order was issued ostensibly to prevent hoarding so that those who take this decades old inexpensive treatment with a long safety record for approved conditions like lupus would have access to it. He later amended the order to allow hydroxychloroquine's use in later stage patients in hospitals, but not in early outpatient treatment. Both hydroxychloroquine and chloroquine had shown efficacy in the prior SARS coronavirus epidemic and studies in France and other countries had already shown its effectiveness for COVID-19, but instead of making research and production of a promising therapy a priority so that there wouldn't be shortages, vents became the near exclusive focus along with the search for a vaccine. This has been true even of President Trump, who despite his public cheering for hydroxychloroquine has not made it the focus of warp speed, funding, and testing. A number of US studies have shown the promise of hydroxychloroquine-based therapies, most recently a Yale University study focused on early treatment. And in what may be the most scandalous retraction in recent memory, a Lancet paper that purported to show hydroxychloroquine alone or with other therapies was in fact dangerous has been shown to be based on fraudulent data. Aaron's home hospital system confirmed in a phone conversation with perspectives on the pandemic that they have used a protocol involving hydroxychloroquine and zinc to great effect. Because in your view this should be an individually decided doctor patient choice. Everything should be that. I mean there is no reason that any government should get in between a doctor patient relationship. That's none of their business. You know if anything is hyperprotective it should be that. I mean when you think about it it's sickening. It's the same reason they won't use like other treatments that are successful around the world and I had a conversation with a doctor about this. Are you guys doing like different sorts of like treatments? Because I know like they have, yeah but I mean there's you know they're coming out with different things that are in the testing. It's a thing they can with a platform that kill more people than actually save. So that's one. And he said that they don't work anyway and I told him well obviously what you guys haven't going on here isn't working. So what's the harm in trying? I don't expect any of these people to survive. 90% of them would die. I mean it's just maintaining. So I figured if it's assumed they're going to die anyway. Just try not throw a few. Well it's you know I don't know that's always an issue in medicine whether you can do it in the bank anyway or not. But if you could find a cure. Well there's no cure. So there's not entire virus therapy. The only way to do it is cure. But treatment I should say rephrase treatment. You could treat it but you know it's you have some scientific basis for whether these things are working or not. A strong everything at them. You could make them worse. So worse than death. Well wait 90% maybe that's a little bit true I don't know. If there's no basis for it working I mean you wouldn't just try to discuss. I would. I might save my life. Yeah. Hello. So with these actual COVID patients they they present by not really being able to breathe. Maybe they've as you say they've probably waited too long. They're not able to breathe in some of that anxiety. And what else do they what how how else do they present? So if they're long. So if you look at their x-rays you can immediately see that these patients are affected by COVID because they're white. Their lungs are white. And the secretions are really really thick. Mucousy and white. And that's what the photo or the extra of these lungs look like. And what so what does a white long look mean? Is that just is that mucous? Yeah it's coded. It's almost like their lungs are coded. So that makes it hard to obviously transfer oxygen into the bloodstream. And so okay so they've got very mucousy lungs and how do you deal with that? Is that what hydroxychloroquine and zinc do? I mean those treatments are for beginning stages. Like once you get to the stage where your lungs are looking like that and you're having a lot of trouble breathing. There are proven treatments that have passed but three trials in Asia through Dr. Cheng. He's a U.S. Board Certified Physician. Is this like extremely high dose IV vitamin C? You successfully treating people with that. And what that's doing is it's giving your body essentially your lungs like the power the antioxidant power to kick it out while you can be getting IV antibiotics to be treating this and getting rid of it. But they don't want to have anything to do with it here. What they want to do is just throw a amount of vent and so they don't have you done the high dose IV vitamin C that's successful in Asia? I have a lot of work with Amy. There's a lot of people trying to find a kind of serious stuff. There's no is this basic providing the city to work in Asia? Well that Dr. Cheng he was the one that it went through the that high dose. I'm talking super high dose IV vitamin C. That's super in an accident. Tell what's your body fight that? It passed three three trials and it's effective. It's just weird how like everybody just like shuts it down immediately. It's very in the right in the C story is in around for a very long time. Oh that's weird because I take it daily and I have a second. It's just a good D. If you're not getting sick I don't think it's done right in the C. It may just a good D. So how quickly how quickly does so if you have a COVID and a COVID rule out or a non-COVID right next to each other on vents will the COVID patient die more quickly than the non-COVID patient? If they're on vents now they're both the same at that point. Yeah. Really? Yeah. So even though the COVID patient with the you know presenting with a very mucousy lung I mean are there lungs filled or they're just coded? I shouldn't say that. I'll take that back. It really depends on the person how healthy they were before. That really determines how long that they're going to be able to sustain the paralytics and you know sedation and multiple different procedures. Even when you're like sleeping or you're like you know knocked out sedated and they're putting you through like these central lines that they're putting in and trakes they're doing trakes even though they're practicing essentially. Your body knows what's going on it's still going through a trauma. It's very traumatic even when you're under. That's why surgery takes while through a cover found because you'll feel it or you know how long do you feel that if you've ever had a surgery and so they're putting in their bodies through their body. They're horrible things and that's adding more stress. It's killing them. So the guy that pulled out his tube is really unique because I saw him from the minute he got to our unit and I didn't agree with him coming to it with ICU but he was admitted with hyperglycemia which is high blood glucose at like 700 so it's pretty high. I learned later that it was high because they were treating him with a lot of different psych drugs and that increases it. It was the treatment that got him to the 700 and when you have a blood glucose that high you're automatically going to have ultra mental status. So now they called him crazy. Okay so he's admitted to the ICU whenever it was like well why is he here because he was acting out. He didn't know where he was. He was confused and I went in there and he wasn't my patient but you know we help each other. I went in there and I tried to talk to him and call him down like hey he's just like I just want to get out of here. I want to get out of here. He has a soft wrist strain son so he's they restrain everybody. We have soft wrist strain son. All of our patients the majority of them for sure which is I think is crazy but it goes with it goes with the territory because everybody's really lazy and it's easier to just treat them with drugs or tie them to their beds. So he was tied up obviously what is that going to do? It's going to make your tie up in a hospital you know having a family what do you think you're going to you're going to freak out. So he was. Lays oxygen was sitting at you know 88 you know 87 doctor comes in I should say fellow comes in and she says that if he can't get his if she goes if you can't get your breathing under control we're going to have to put a tube in you to help you with that and I go what I'm like he doesn't need it to down his throat like he doesn't need a vent she goes well yeah he's he's de-sad and I said no like absolutely not he does not need that we need to get his blood sugar under control and he will be fine and maybe not tied to this bed and she goes yeah we'll talk about it we'll we'll just bondage her hand and this was I was working night shift this was probably around 6 am at quarter of a sudden we had a cold down the hall did the the cold past had to do all that got out of there I come back for a shift and guess what the guy has been on a vent I was so upset they did it I guess the the nurses that took over said they did it literally as I left so I come back in the morning he's on a vent yeah like you have to be kidding me he did not need a vent the way it is for you to leave they did we literally we literally that was the morning we coded 28 for three minutes that we know sin are tipped at that other than that room cleaned it and put it in here yeah a tube cover yeah they took his vent at our he died they put it on him so they waited until I left because they know how I feel about this so same thing with that nine they didn't need to intubate him he was progressing I don't think that he I don't know what happened after we tried by that and then they've brought him here and I thought well cross my fingers see no one survives he did he was the only one that I've had this happened with him because of his two though and so he has a chance again oh he did it excitated himself oh he did I didn't know that I thought he was exterated and how did he wake up turns out that he did drugs so he was resistant he was to fentanyl all of this stuff that we get normal people didn't put it for him so he ended up yeah I'm like you just say oh I'm like you just saved your own life you know that's crazy don't know what that is but I needed it you know it's sad so he pulled it out and they're like oh you know so and so it's exterated and I'm like no way they don't exterate anybody I'm like that's so weird here it turns out he's exterated himself and now he I mean he's fine he's home now this was this a couple days ago but you know what's sad is that he thinks we saved his life you know what I mean so he's like you saved me and I I couldn't you know I don't have the heart to be like no man you saved yourself you have like nine lives because had he had you not pulled that out he would definitely he would definitely be that for sure they don't exterbate anyone here the problem not a presentation here since this thing began has been this charge or successfully exterated I asked the nursing supervisor for a sitter for the guy that pulled this tube out because when they're waking up they can be they can be extra I should say where they need a little bit of extra attention and I asked her for a sitter and she told me that I didn't utilize all my resources first which was held all all the psych drugs to like chemically chemically you know put him to bed the your Florida hospital was literally having to furlough people yes what was happening is obviously they shut down all elective procedures but they were also waiting for the wave they called it the wave so we were preparing and we were in tears based on our experience so we were tier one tier two tier three tier four and I was tier one because I have the you know military trauma experience I see your experience so on so forth so I was working you know throughout the hospital training and other units cross training um ultimately it was two hours you know it was what there's to get hours yeah yeah this is what the hospitals were doing they're like okay we're gonna give our employees hours this way to cross train them for when the wave hits and then that wave would get pushed back another week and then they get pushed back another week and the units that we were floating to like cross training they're like what are you doing here we don't need you you know so I felt like I was wasting my time and taking out other other people's time that we're trying to get hours too and this opportunity presented itself and I took it do you think that the reason you never got a COVID wave in Florida was because of any of this lockdown or I mean what I mean I mean I know you're not an epidemiologist but what do you think what's going on I am I live right by and that was like worldwide news people were at the beach I was one of those people at the beach with my kids some like it's vitamin D it's good for your immunity fresh air salt water all these things are really good for anyone's and you know immune system you have to be out mental hell you know we were all at the beach and so people if there was a lot of transmission going on when you think our hospitals would be flooded they're not I'm right at the beach I'm right by the beach didn't happen because the lockdowns happened after all that and it was spring break you know the beaches were bad I mean there's people from all over the world they were people are all I mean tons of New Yorkers lived by us what do you what do you if you I know I'm asking you to speculate here because you you really feel there is something a new disease called COVID-19 a new do you feel that that's the case or do you think that this is I mean I know there's a lot of mislabeling and I know all that and but there really is something new right and so okay yeah okay and and how what why do you think it places like New York got well okay we can see that what you were describing at Elmer's was that they were packing people in together and so that would cause spread but what why do you think the place like the New York got hit so much harder than other places I thought about that already what I found is that before this happened does it did make sense to me I'm like I'm sitting at home I'm waiting for work I'm stressing out a lot of my friends are doing the same so I'm like digging in like why is New York like what is it because there's that many people crunched in together but ultimately what I found is that the hospitals here were already struggling and I think they shut down like multiple hospitals because they couldn't afford to keep them open so that made sense to me even though I didn't want it to make sense you know like there's really no other I'm a reason because like but do you think we have do you think we really do have many more cases regardless of whether or not you know people went to the hospital um I think they're forced cases I mean sure people are coming in with COVID whatever that may be it is something but not everyone but they're admitting these people that's the difference between New York hospitals or these you know Michigan you know the states that were you know hit the hardest quote um they're admitting these patients as possible COVID calling it COVID or rule out COVID rule out COVID when they maybe just had a little congestion if there was something you would want to tell everyone in the country and everywhere else what what one last thing what would it be yeah I would say this is this is the one thing that I've had a struggle with is if someone like me or anybody is trying to tell you something that might go against your beliefs like just listen you know like really just take it in and instead of jumping on it like think on it for a night or a day like look into this stuff because and ask people about it um like not every nurse is going to have the same experience a med surgeon or a sets on the floor even in my own hospital has not had the same experience as the ICU nurses have and once I sit down and explain it to them it all makes sense they're like yeah that makes sense we see that because we'll send them to your you know also just like just think about it you know and and be very very respectful and like they're we don't want to I don't know when wants to put themselves in a situation like this you know and it's really hard and this is the reason that a lot more people and nurses are afraid because people are so quick to you know defend something that they don't really understand what are you referring to particularly like this protocol or what like I referred to earlier if you tell people like something and not over and over like the media was telling people you know vents vents vents vents and then you say as a nurse no vents you know it's not a good it's not a good position to be in because I'm going against what the government says but does the government really have everybody's best interest in mind you know are they thinking of you know the 57-year-old grandma that you know wasn't didn't have to die or the 37-year-old that was totally fine when he walked into the emergency room and he didn't have to die you know are they thinking about you know maybe the guy that had a drug problem that didn't have to be invented but he saved his own life I don't have anything to gain and I have everything to lose by cheering when I'm cheering right now you know but so be it you know I think it's important that these families get closure and I hope that someday they'll be able to you know you know hold them accountable for what they did a few days after we recorded this interview Aaron began to feel that her time at Elmhurst was drawing to a close her vocal questioning of hospital procedure and her efforts to get the word out on social media were getting noticed she made this recording on what ended up being her last day at the hospital I've been taking care of a patient for like a week right now and this is my **** and I call them and he's been doing great he had a trick put it in he's been doing great he's been talking like her communicating with me he's telling me like laughing at my jokes and talking to his kids on FaceTime a couple days ago and I told him that he was doing fine and he was today I was giving him and they came in and they told me that I need to leave the room and they have to give report to somebody else they took me from that unit they put me in the emergency room they don't need me there but they put me there and I'm not even there like 20 minutes not even there 20 minutes and I hear a cold being called in my room that I was just laughed and it's him and he was fine he was fine I don't understand and nothing makes sense like why would they take me out of his room and put me in the heady and then not 20 minutes later he's dead it doesn't make sense like did they kill him he was my one patient that was gonna live he shouldn't have died I don't know what they did to him something's not right the only reports that we're able to get what's going on are coming from the inside and people are afraid to speak out people have lost their jobs do not give consent for intubation if you don't want to be intubated or your loved one to be intubated demand non-invasive or less invasive ventilation methods soon as you give that consent you might not come out of it now in some cases it might be appropriate we just don't know we know that it's being used inappropriately in a lot of cases and that the ventilators are making people worse the ventilators are making people worse the ventilators are making people worse the ventilators are to this war what missiles were to world war two do with 400 ventilators when I need 30,000 do with 400 ventilators when I need 30,000 look at mortality those aged 18 to 65 years of age and those greater than 65 years of age those who are on no vent and those that are on the vent or had to be on the vent mortality rate for those 18 to 65 not on the ventilator was 19.8% those greater than 65 26.6% on the ventilator between 18 and 65 years of age 76.4% those on the ventilator greater than 65 years of age a whopping 97.2% mortality based on this data those on the ventilator greater than 65 years of age a whopping 97.2% mortality those on the ventilator greater than 65 years of age a whopping 97.2% mortality in brainwash to think they're doing something great just by going to work because they're brave enough to go to work well what are you doing at work you're certainly not saving people if you're you're not even running codes you're not even going into patient rooms you're a coward you're hurting people you're killing them you're contributing to the problem I know I'm going to get hate mail for this and that's fine because people are dying who don't have to die again there's no family there so no one's being held accountable and once these people get intubated they're being scared into giving consent to be intubated and then for a lot of them it's over and there's nobody going to be held accountable and there's nobody looking out for them they are completely by themselves again there's no family there so no one's being held accountable and once these people get intubated they're being scared into giving consent to be intubated and then for a lot of them it's over they're being scared into giving consent to be intubated and then for a lot of them it's over they're not heroes we're gonna be held away we're gonna turn to understand you're gonna tell the first they're being scared into giving consent to be intubated and then for a lot of them it's over and is asking for more medical equipment by early April we need three million and 95 masks we need 50 million surgical masks we need 15,000 ventilators he's also requesting 25 million each of surgical gowns coveralls gloves and face why would they take me out of his room and put me in the heady and then not 20 minutes later he's dead it doesn't make sense like did they kill him? does it make sense? like did they kill him? did they kill him? did they kill him?





 Donate
Donate